Blog Categories
Achilles tendon
4Posts
Acl
4Posts
ACL tears
3Posts
Ankle injury
7Posts
Ankle sprains
4Posts
Back
5Posts
Back pain
12Posts
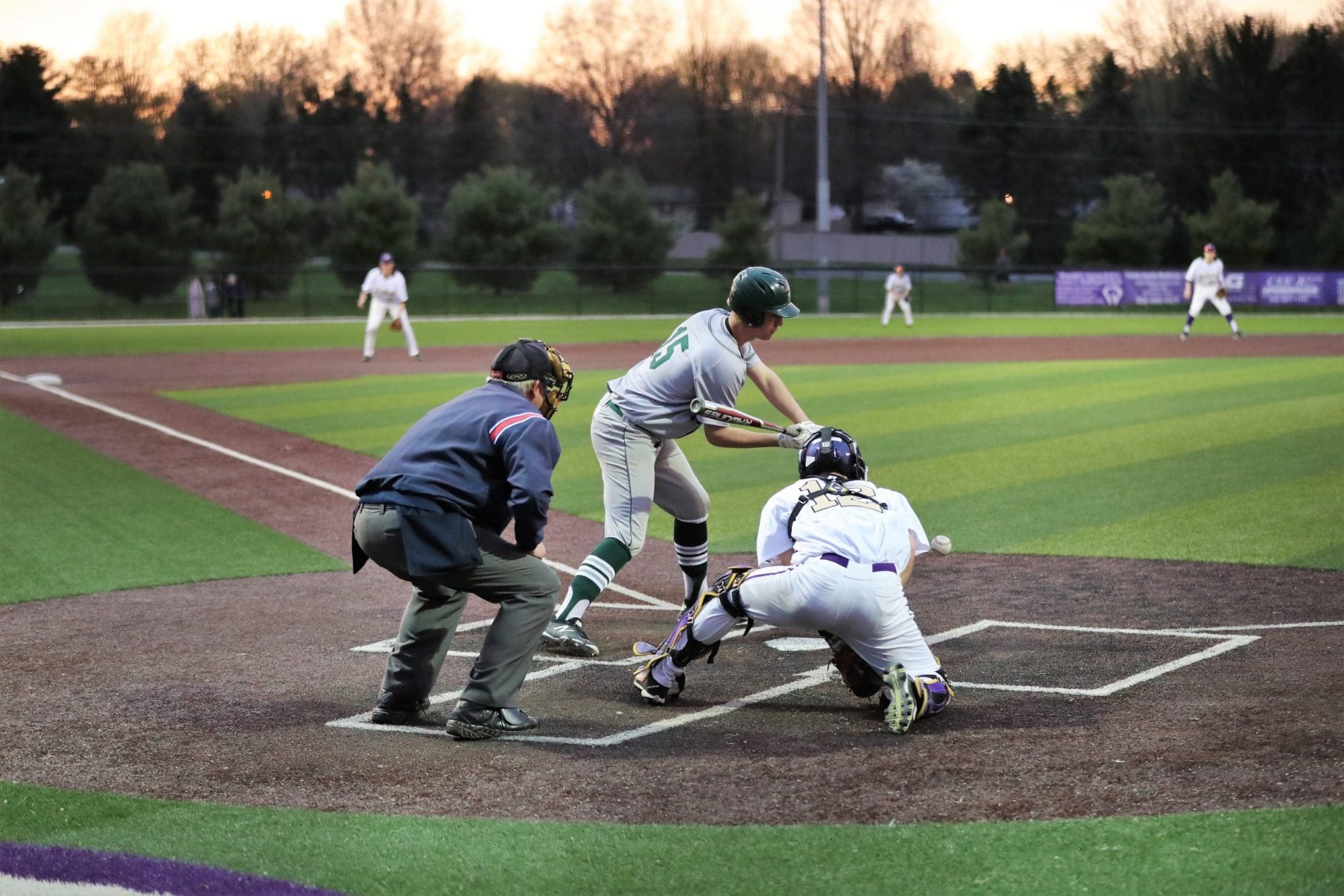
Baseball
2Posts
Breast cancer
1Posts
Chiropractor
2Posts
Community
1Posts
Concussion
22Posts
Cycling
1Posts
Elbow
1Posts
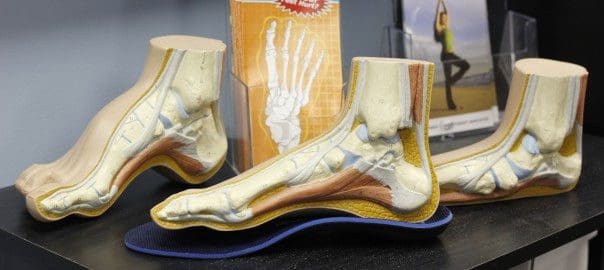
Feet foot
3Posts
Foam roller
1Posts
Glutes
3Posts
Golf
7Posts
Hamstring or calf
1Posts
Hamstring strains
2Posts
Head injuries
7Posts
Hernia
1Posts
Hockey
2Posts
Injuries
3Posts
Injury Management
7Posts
Injury prevention
66Posts
Injury recovery
27Posts
Injury treatement
26Posts
Knee
5Posts
Larsen-Johansson (LJ)
2Posts
Lower back injury
4Posts
Massage therapy
3Posts
Mental Health
1Posts
Mental illness
1Posts
Mental image
1Posts
Muscle tear
2Posts
Muscles
7Posts
Myofascial release
1Posts
Neck
3Posts
News Articles
136Posts
office exercises
6Posts
Old
1Posts
OSC
1Posts
Osgood Schlatters (OS)
2Posts
Osteoarthritis OA
1Posts
Pain
8Posts
Pain understand
1Posts
Performance
10Posts
Physical Therapy
11Posts
Preparation
6Posts
Rehabilitation
6Posts
Repetitive Strain Injury
1Posts
Reputation
2Posts
Rugby
1Posts
Running
10Posts
Sciatica
3Posts
Severs disease
2Posts
Shoulder
5Posts
Shoulder pain
2Posts
Ski
2Posts
Snowboarding
1Posts
Soccer
10Posts
Spine
1Posts
Sport Doctor
6Posts
Strength
6Posts
Stretch
1Posts
Swimming
3Posts
Teenagers
3Posts
Uncategorized
4Posts
Vertigo
1Posts
Warm up maintain
1Posts
Warm up with ice
1Posts
Winter injuries
3Posts


February 24, 2017


January 28, 2016